McMaster researchers identify how VITT happens
A McMaster University team of researchers has found how, exactly, the COVID-19 vaccines that use adenovirus vectors trigger a rare but sometimes fatal blood clotting reaction called vaccine-induced immune thrombotic thrombocytopenia or VITT.
The findings will put scientists on the path of finding a way to better diagnose and treat VITT, possibly prevent it and potentially make vaccines safer.
Their article was fast-tracked for publication today by the prestigious journal Nature in its accelerated article preview because of the importance of the research.
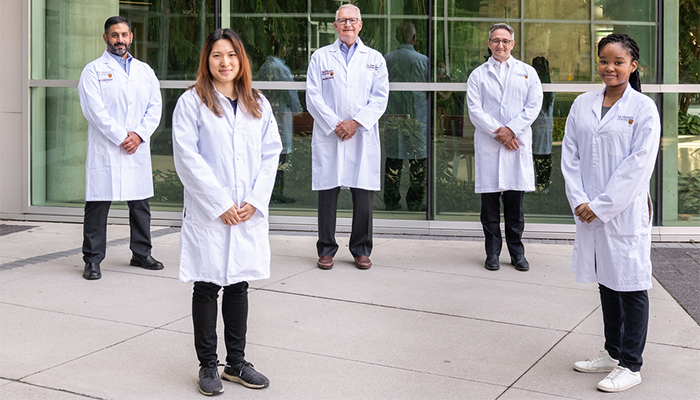
“Our work also answers important questions about the connection between antibodies and clotting,” said Ishac Nazy, principal investigator and corresponding author of the study. He added it will have both diagnostic and therapeutic implications.
Nazy is the scientific director of the McMaster Platelet Immunology Laboratory and an associate professor of medicine for the Michael G. DeGroote School of Medicine at McMaster.
The COVID-19 vaccines using adenoviral vectors, such as those from AstraZeneca and Johnson and Johnson, are associated with the VITT clotting disorder caused by unusual antibodies to blood platelets that are triggered by the vaccine.
The study shows, at a molecular level, how those unusual antibodies stick to components from blood platelets causing them to trigger clot formation.
“The antibodies stick to the platelet protein called platelet factor 4 (PF4) in a very unique and specific orientation, which allows them to align with other antibodies and platelets in the precise formation that leads to a self-perpetuating vicious cycle of clotting events,” said Nazy.
“These disease-causing aggregates quickly activate platelets, creating a highly intense clotting environment in patients,” he added.
The dangerous reaction to the adenovirus vector vaccines has been found to occur in one in 60,000 of people receiving the vaccine in Canada.
“The intention of our study was to better understand how the severe clots which characterize VITT develop,” said Donald Arnold, study co-investigator and co-medical director of the McMaster Platelet Immunology Laboratory.
“A basic principle of medical care is to understand how the disorder happens and, in doing so, develop better treatments.”
John Kelton, co-investigator of the study and co-medical director of the McMaster Platelet Immunology Laboratory, added: “We believe that this study is important because it clarifies how the clotting ensues, and because we have been able to identify the molecules involved.
“The next step is to develop a rapid diagnostic and accurate test to diagnose VITT. Our major interest is now to move upstream from how the clots happen to preventing them from occurring.”
Current rapid tests yield false-negative results, and testing relies on more time-consuming tests to confirm VITT. This study now explains why the rapid tests frequently fail and allows for new strategies to improve diagnostic testing.
The investigators altered the molecular composition of the PF4 protein and, using this technology, were able to identify the binding region on the protein.
The research team included Angela Huynh, a research scientist in the McMaster Platelet Immunology Laboratory, and Mercy Daka, a graduate student of McMaster’s Department of Biochemistry and Biomedical Sciences.
The researchers thanked the agencies supporting the research, including the Public Health Agency of Canada, the Canadian Institutes of Health Research (CIHR), and the Ontario Ministry of Health.
A link to the article may be found here
Research Findings
